OrthoEdge — El Paso Sports Medicine & Orthopedic Surgery
Return Strong. Play Hard. Live Pain-Free
Welcome to OrthoEdge!
William Arroyo, MD
Dr. William Arroyo is a board-certified orthopedic surgeon with subspecialty training in sports medicine. He is dedicated to the treatment of shoulder, knee, and hip injuries, offering patients the most advanced options in arthroscopic and minimally invasive surgery. His expertise includes complex reconstructive procedures, ACL reconstruction and meniscus repair, rotator cuff surgery, and cartilage restoration. In addition, Dr. Arroyo performs joint replacement surgeries, specializing in knee and shoulder replacements, utilizing the latest techniques and technologies to optimize recovery and long-term outcomes. With a strong commitment to patient care, he combines surgical precision with personalized treatment plans to help athletes and active individuals return to their highest level of performance.
Diplomate, American Board of Orthopedic Institute.
Double Board Certified in General Orthopaedic and Sports Medicine.
Fellow, American Academy of Orthopaedic Surgeons.
Fellow, Arthroscopy Association of North America.






Comprehensive surgical and non-surgical care for athletes and active adults.
Advanced minimally invasive techniques, personalized rehabilitation, and faster, safer recoveries.
Sports Medicine
Shoulder, Knee, and Hip Arthroscopy
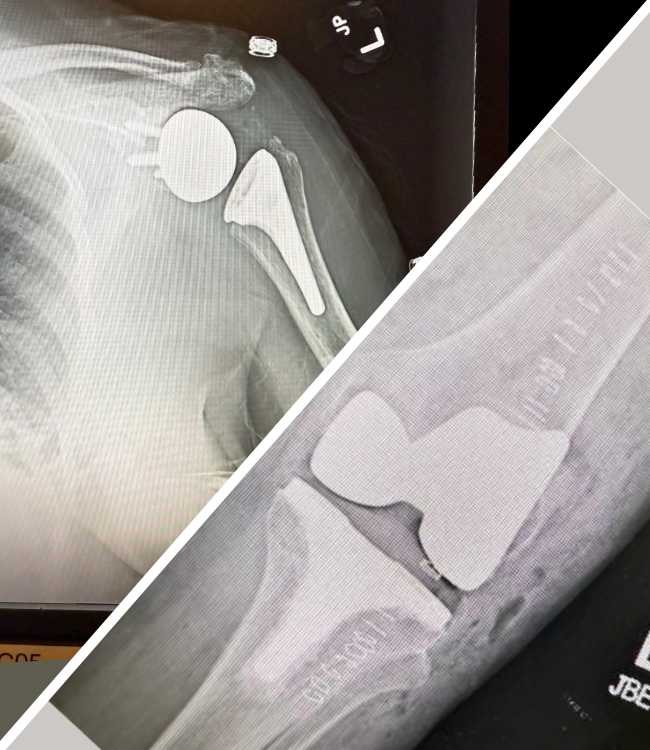
Knee and Shoulder Replacement Surgery
Advanced Fracture Management
Platelet-Rich Plasma (PRP) Injections
Bio-Active Peptides Treatment
Men’s Wellness
I Specialize in Knee and Shoulder Replacement Surgery.
What is joint replacement? Joint replacement is a surgical procedure that removes damaged or worn portions of a joint and replaces them with durable medical-grade components to restore pain-free movement, stability, and function. For people whose arthritis, injury, or deformity no longer responds to non-surgical care, joint replacement is a proven option to dramatically reduce pain and improve daily activities.


Benefits Patients Can Expect.
- Lasting and substantial pain relief
- Improved range of motion and joint stability
- Faster return to normal daily activities
- Improved quality of life
- Long‑lasting results with modern implants and surgical techniques
Who is helped by replacing the Shoulder or Knee.
- Patients with joint osteoarthritis, rheumatoid arthritis, severe rotator cuff arthropathy, avascular necrosis, or complex fractures of the shoulder joint.
- People with persistent joint pain, stiffness, and loss of overhead function that limit work, sports, or daily living.
What the surgery does:
- Removes the damaged surfaces of the joint replaces them with prosthetic components designed to restore smooth, pain-free gliding and rotation.
Arthroscopy
William Arroyo, MD, an experienced, patient-centered arthroscopic surgeon offers advanced minimally invasive care for shoulder, knee, hip, and ankle conditions.
What is arthroscopy?
Arthroscopy is a minimally invasive surgical technique that lets orthopedic surgeons see, diagnose, and treat problems inside a joint using a small camera (arthroscope) and specialized instruments. Instead of a large incision, the surgeon makes small keyhole openings to insert the camera and tools. The camera projects high‑resolution images onto a monitor so the surgeon can precisely repair or remove damaged tissue.

Hip Arthroscopy
Why Choose It: Ideal for addressing hip pain and dysfunction without a large incision, hip arthroscopy can help preserve the hip joint, improve range of motion, and alleviate pain, particularly in younger, active individuals.

Shoulder Arthroscopy
Advantages: It offers a less invasive alternative to open shoulder surgery, resulting in smaller scars, reduced post-operative pain, and a generally faster return to activity for many patients.

Knee Arthroscopy
Benefits: Often performed as an outpatient procedure, knee arthroscopy allows for quicker recovery and less pain compared to traditional open surgery, helping you get back on your feet faster.
Why you should choose OrthoEdge.
OrthoEdge provides comprehensive orthopedic surgical and non‑surgical care focused on restoring mobility, reducing pain, and improving quality of life. Dr. Arroyo offers advanced, evidence‑based procedures for injuries and degenerative musculoskeletal conditions, using minimally invasive techniques and personalized care plans that prioritize safe recovery and optimal functional outcomes.
Year of Experience

5 Star Client Rating

Your Title Board-certified orthopedic surgeon with fellowship training in joint reconstruction and sports medicine Here
Strong emphasis on individualized perioperative care, multimodal pain control, and rehabilitation planning
Skilled in complex fracture management and soft-tissue reconstruction after trauma
Proficient in minimally invasive and arthroscopic techniques to shorten recovery and reduce scarring
Extensive experience with primary and revision total joint arthroplasty using modern implants and navigation technologies
Active in outcomes-driven practice, patient education, and adoption of evidence-based protocols to optimize functional results
Seeking Professional Help Is Not a Weakness
How can surgery help you?
Accurate Diagnosis
pinpoint the issue fast so you get the right treatment.
Step 01
Faster Recovery
tailored surgical or non-surgical plans speed healing.
Step 02
Pain Relief
Proven procedures and therapies reduce or eliminate pain.
Step 03
Restore Function
Step 04
Frequently asked questions and answers
“How much pain will I be in after the surgery, and how will it be managed?”
“It’s completely normal to have some pain after surgery, but our primary goal is to manage it effectively so you can be as comfortable as possible. We use a multi-modal approach, which means we’ll likely use a combination of medications, including oral pain relievers, and sometimes nerve blocks or other techniques, depending on the type of surgery. We’ll also encourage non-pharmacological methods like ice, elevation, and proper positioning. We’ll monitor your pain levels closely and adjust your medication as needed. Please don’t hesitate to tell us if you’re uncomfortable.”
“How long will it take for me to fully recover and get back to my normal activities, like work or sports?”
“Recovery time varies significantly depending on the specific surgery, your overall health, and how diligently you follow your rehabilitation plan. For many orthopedic procedures, we’re looking at several weeks for initial healing, and then several months for a more complete return to full activity. For example, a knee replacement might mean 6-12 weeks until you’re walking comfortably, but 6 months to a year for full strength and endurance. We’ll work together with your physical therapist to set realistic goals and a phased return to your activities. While our aim is to restore as much function as possible, ‘normal’ might feel a bit different, but often significantly better than before surgery.”
“What are the potential risks or complications of this surgery?”
“It’s important to be aware of the potential risks, and we take every precaution to minimize them. Common risks for most surgeries include infection, bleeding, blood clots (DVT), and adverse reactions to anesthesia. Specific to orthopedic surgery, there’s also a small risk of nerve damage, implant loosening (if applicable), or delayed healing. While these complications are rare, we’ll discuss them in detail during your consent process. We have protocols in place to prevent these issues, and we’ll monitor you closely both during and after the procedure. Please ask if any of these concerns you.”
“Will I need physical therapy, and how important is it to my recovery?”
“Yes, for almost all orthopedic surgeries, physical therapy (PT) is absolutely crucial – it’s often as important as the surgery itself. The surgery fixes the structural problem, but PT helps you regain strength, flexibility, balance, and proper movement patterns. It prevents stiffness, builds muscle around the surgical site, and teaches you how to safely use your newly repaired joint or limb. Skipping or not fully committing to PT can significantly compromise your long-term outcome and increase your risk of re-injury. Your physical therapist will guide you through exercises tailored to your specific needs, and we’ll monitor your progress closely.”
“What should I expect immediately after surgery, when I wake up?”
“When you wake up, you’ll be in the recovery room. You might feel a bit groggy or disoriented from the anesthesia, which is normal. You’ll likely have some discomfort, but we will have already started your pain management, so it should be manageable. You might have dressings on the surgical site, and possibly a drain or an IV line. Our nurses will be right there with you, monitoring your vital signs, pain levels, and making sure you’re comfortable. We’ll keep you updated on how you’re doing and when you can expect to move to your hospital room or prepare for discharge.”
“What kind of restrictions will I have after surgery, and for how long?”
“You will definitely have some temporary restrictions to protect the surgical site and allow for proper healing. These will be very specific to your procedure. For example, you might have weight-bearing restrictions (e.g., no weight on your leg for a few weeks), limitations on lifting, or restrictions on certain movements (like bending or twisting). Driving is typically not allowed while you’re on strong pain medication or if your mobility is impaired, often for several weeks. We’ll provide you with a detailed list of ‘do’s and don’ts’ before you go home, and your physical therapist will reinforce these. It’s vital to follow these restrictions carefully to prevent complications and ensure the best possible outcome.”
“How do I know if something is wrong after I go home, and who should I contact?”
“We’ll give you clear instructions on what to watch out for. Generally, you should contact us immediately if you experience a sudden increase in pain that isn’t relieved by your medication, a high fever (over 101°F or 38.3°C), significant redness, swelling, or pus coming from the incision site, or any numbness or tingling that wasn’t present before. For less urgent questions, our office will have specific hours, but for emergencies, you’ll have an after-hours number to reach the on-call doctor, or you should go to the nearest emergency room. We want you to feel secure and know that we’re here to support you through your recovery.”

Recent articles and latest blog
There are many variations of passages of Lorem Ipsum available, but the majority have suffered alteration in some form, by injected humour, or randomised words.


